Overview Ichthyosis
Ichthyosis is a group of rare, genetic skin disorders characterized by dry, scaly skin that resembles fish scales. It’s a form of dry skin. The condition results from mutations affecting the skin’s ability to shed dead cells, leading to thickened, flaky patches. While some forms of ichthyosis are inherited and present from birth, others may develop later in life due to external factors or medical conditions. The severity of symptoms can vary widely, ranging from mild dryness to severe scaling that impacts quality of life. Although there is no cure, treatments like moisturizers, exfoliating agents, and specific therapies can help manage the condition effectively.
What are the Symptoms of ichthyosis?
- Dry, flaky skin that may resemble fish scales
- Thickened patches of skin
- Cracking of the skin, which may lead to discomfort or infections
- Redness or inflammation in affected areas
- Itchiness or irritation
- Difficulty with skin shedding, resulting in built-up scales
- Sensitivity to cold or heat due to impaired skin barrier function
- Nail abnormalities, such as thickening or ridges
- Difficulty sweating, leading to overheating in hot weather
- Eye-related symptoms like redness, irritation, and increased tearing if ichthyosis affects the eyelids.
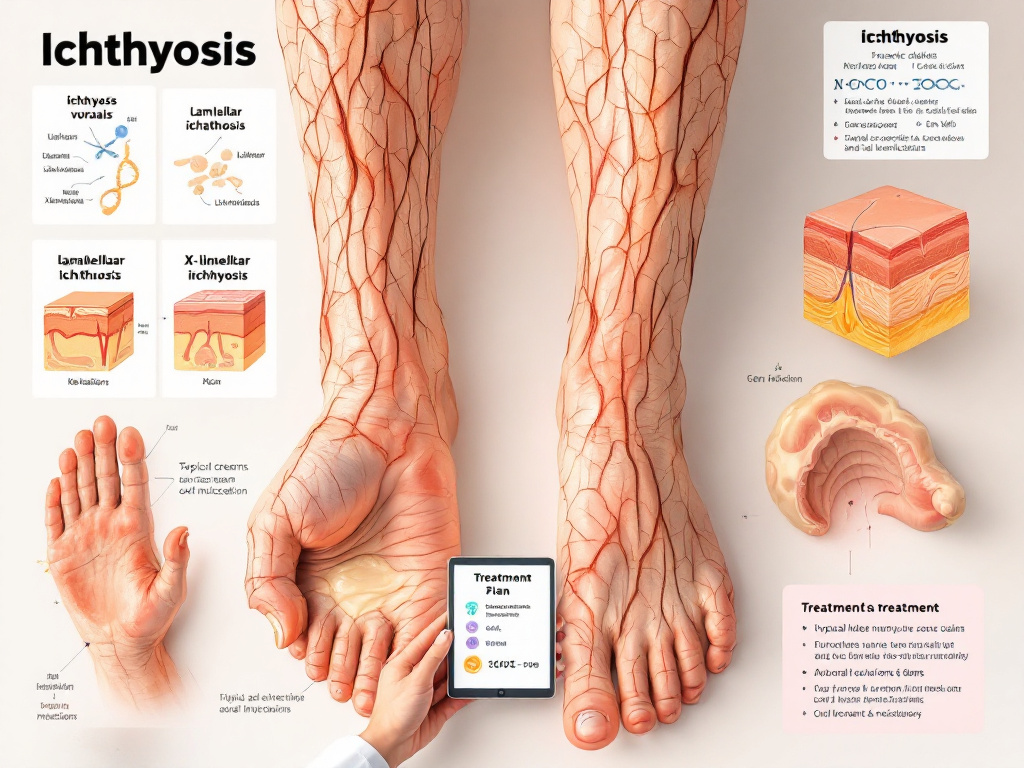
What are the types of Ichthyosis?
There are 10 types of Ichthyosis.
- Ichthyosis Vulgaris
- Lamellar Ichthyosis
- Harlequin Ichthyosis
- X-Linked Ichthyosis
- Congenital Ichthyosiform Erythroderma (CIE)
- Epidermolytic Ichthyosis (EI)
- Acral Peeling Skin Syndrome (APSS)
- Ichthyosis Hystrix
- Netherton Syndrome
- Syndromic Ichthyoses
Explanation of all types
1. Ichthyosis Vulgaris
Ichthyosis vulgaris is the most prevalent form of ichthyosis, often inherited in an autosomal dominant pattern. It typically manifests in early childhood, causing areas of dry, scaly skin, particularly on the arms, legs, or back.
The condition arises due to mutations that damage the skin’s natural ability to shed dead cells, leading to the buildup of scales that trap moisture. Symptoms may become more pronounced in colder climates when the air is dry, while they often improve in humid environments.
2. Lamellar Ichthyosis
Lamellar ichthyosis is a rare genetic condition inherited in an autosomal recessive pattern. It is present from birth and often leads to the appearance of thick, plate-like scales that cover large areas of the body. These scales can range in color from brown to gray and are surrounded by deep fissures, which may cause discomfort or increase the risk of skin infections.
Lamellar ichthyosis results from mutations affecting the skin’s ability to produce a healthy barrier, leaving it dry and prone to irritation. Individuals with this condition may also experience difficulty regulating their body temperature due to impaired sweating.
3. Harlequin Ichthyosis
Harlequin ichthyosis (HI) is a rare, genetic disorder that causes thick, hard skin to form in large diamond-shaped plates, separated by, often This condition is inherited in an autosomal recessive pattern, often evident at birth. The thickened skin can severely limit movement and affect the flexibility of joints, eyelids, nose, and mouth.
The condition arises due to mutations in the ABCA12 gene, which plays a critical role in skin development. Infants with harlequin ichthyosis face significant challenges, including difficulty maintaining body temperature, risks of dehydration, and increased susceptibility to infections due to the compromised skin barrier.
5. X-Linked Ichthyosis
X-linked ichthyosis is a rare genetic skin condition that mostly affects males because it’s passed down in an X-linked recessive pattern It’s caused by mutations in the STS gene leading to a lack of the steroid sulfatase enzyme, which is important for breaking down certain lipids in the skin.,.
Individuals with X-linked ichthyosis often exhibit dark, thick scales, typically found on the neck, arms, torso, and legs. Unlike other forms of ichthyosis, the face, palms, and soles are generally unaffected. Symptoms usually manifest shortly after birth or in early childhood and persist throughout life.
6. Congenital Ichthyosiform Erythroderma (CIE)
Congenital Ichthyosiform Erythroderma (CIE) is a rare genetic skin disorder inherited in an autosomal recessive pattern. It is present at birth and is characterized by widespread, diffuse redness of the skin (erythroderma), accompanied by fine, white scales that may cover large areas of the body.
The condition results from mutations in genes responsible for maintaining the skin barrier, leading to excessive dryness and scaling. Individuals with CIE often experience symptoms such as tightness of the skin, which can restrict movement, and an increased risk of skin infections due to compromised skin integrity.
7. Epidermolytic Ichthyosis (EI)
Epidermolytic ichthyosis (EI) is a rare genetic skin disorder inherited in an autosomal dominant pattern. It is characterized by severe dry, scaly skin, often accompanied by blistering and redness. The condition typically presents at birth or in early infancy, with affected individuals frequently experiencing fragile skin that is prone to splitting and infections.
EI arises from mutations in keratin genes, which disrupt the structure of skin cells, leading to a weakened skin barrier.
8. Acral Peeling Skin Syndrome (APSS)
Acral Peeling Skin Syndrome (APSS) is a rare genetic skin condition inherited in an autosomal recessive pattern. It is primarily characterized by the painless peeling of the top layer of skin on the hands and feet, often exacerbated by exposure to water or friction.
The condition is caused by mutations in genes involved in skin cohesion, which weaken the bonds between skin layers, leading to easy separation. While APSS generally does not cause pain, affected individuals may experience skin sensitivity and occasional irritation. The condition typically appears at birth or early childhood and is usually limited to acral areas, leaving other parts of the body unaffected.
9. Ichthyosis Hystrix
Ichthyosis hystrix is a rare, inherited skin disorder characterized by thick, spiny scales that resemble porcupine quills. This condition is typically inherited in an autosomal dominant pattern and presents with hyperkeratosis, a significant thickening of the skin’s outer layer.
The spiny scales are often localized to specific areas of the body, such as the extremities or torso, and may vary in severity. While the disorder does not usually affect overall health, individuals with ichthyosis hystrix may experience discomfort, restricted movement, or increased susceptibility to skin infections.
10. Netherton Syndrome
Netherton syndrome is a rare genetic condition that affects the skin, hair, and immune system and is passed down in an autosomal recessive pattern. This condition is caused by mutations in the SPINK5 gene, leading to the production of defective proteins involved in skin barrier function and immune regulation.
Individuals with Netherton syndrome often present with red, scaly skin (ichthyosis-like erythroderma), recurring skin infections, and characteristic bamboo-like hair shaft abnormalities known as trichorrhexis invaginata. The compromised skin barrier makes those affected more vulnerable to allergens and infections, while immune dysfunction can lead to severe allergic reactions, including food allergies and asthma.
Symptoms typically appear at birth or within the first few months of life, requiring lifelong management and careful skin care.
11. Syndromic Ichthyoses
Syndromic ichthyoses refer to a group of rare genetic disorders characterized by generalized scaling, hyperkeratosis, dry skin, itching, redness, and cracking. The scales can vary in color, including shades of white, gray, or brown, and often affect large areas of the body. These conditions are usually associated with additional systemic symptoms or abnormalities, such as developmental delays, immune dysfunction, or metabolic disorders.
What are the Causes of Ichthyosis?
There are many causes of Ichthyosis but I have covered some causes.
- Genetic Mutation
- Deficiency of Enzymes
- Keratin Defects
- Impaired Skin Cohesion
I have covered all these causes in FAQ format. After reading, I hope you will learn more about the causes of Ichthyosis.
1. What Genetic Mutation Causes Ichthyosis?
Ichthyosis is primarily caused by genetic mutations that affect the formation and function of the skin barrier. These mutations often occur in genes responsible for keratinocyte differentiation, lipid metabolism, or skin cohesion. For example:
- X-linked ichthyosis is caused by mutations in the STS gene, leading to a deficiency of the steroid sulfatase enzyme.
- Congenital Ichthyosiform Erythroderma (CIE) is associated with mutations in genes such as TGM1, ALOX12B, or ALOXE3, which are important for lipid processing and skin barrier function.
- Epidermolytic Ichthyosis (EI) results from mutations in KRT1 or KRT10 genes, which code for keratin proteins essential for the structural stability of the skin.
- Acral Peeling Skin Syndrome (APSS) involves mutations in genes like TGM5, which play a role in skin adhesion and integrity.
- Netherton Syndrome is caused by mutations in the SPINK5 gene, disrupting proteins involved in skin barrier maintenance and immune regulation.
- Ichthyosis Hystrix is linked to mutations in keratin-related genes, though the specific mutations are less commonly defined.
2. What Deficiency of Enzymes Causes Ichthyosis?
Certain types of ichthyosis are linked to enzyme deficiencies that disrupt normal skin barrier function and cell turnover. For instance:
- X-linked ichthyosis is caused by a deficiency of the steroid sulfatase enzyme due to mutations in the STS gene, leading to an accumulation of cholesterol sulfate in the skin, which impairs skin shedding.
- Harlequin ichthyosis, though not directly due to enzyme deficiency, involves defects in genes like ABCA12, which impact lipid transport in the skin, indirectly affecting enzymatic processes involved in lipid metabolism.
- Congenital Ichthyosiform Erythroderma (CIE) and Lamellar Ichthyosis (LI) can involve deficiencies in enzymes related to lipid processing, such as transglutaminase 1 (TGM1), which is crucial for forming the skin’s lipid barrier.
These deficiencies highlight the critical role enzymes play in maintaining skin integrity and renewal.
3. Is Keratin Defects a Cause of Ichthyosis?
Yes, keratin defects can cause certain types of ichthyosis. Mutations in keratin genes, such as KRT1 and KRT10, are directly associated with Epidermolytic Ichthyosis (EI). These genes encode keratin proteins that play a critical role in maintaining the structural integrity and stability of the skin’s outer layer.
Defective keratins lead to weakened connections between skin cells, resulting in skin fragility, blistering, and the buildup of thickened, scaly skin. The structural abnormalities caused by keratin mutations disrupt normal skin barrier formation, making affected individuals more prone to infections, irritation, and discomfort. Thus, keratin defects are one of the key factors contributing to the pathology of certain ichthyoses.
4. Is Impaired Skin Cohesion a Cause of Ichthyosis?
Yes, impaired skin cohesion is a significant cause of certain types of ichthyosis. Skin cohesion relies on the proper attachment of skin cells through proteins and lipids that form a stable and cohesive barrier. Mutations in genes responsible for maintaining skin cohesion can lead to compromised integrity of the skin’s outer layer.
For example, Acral Peeling Skin Syndrome (APSS) is caused by mutations in the TGM5 gene, which disrupts the adhesion between skin cells, resulting in peeling and fragile skin. Similarly, mutations affecting proteins involved in the stratum corneum lipid matrix, such as those in CIE or Lamellar Ichthyosis (LI), reduce cohesion, causing scaling, cracks, and increased skin permeability.
Though not directly due to enzyme deficiency, Harlequin ichthyosis involves defects in genes like ABCA12. These genes impact lipid transport in the skin, indirectly affecting enzymatic processes involved in lipid metabolism.
What is the Best Treatment of Ichthyosis?
The management of ichthyosis focuses primarily on symptom relief and improving skin barrier function. Treatment factors include the following:
- Emollient and Moisturizer
- Keratolytic Agents
- Bathing and Exfoliation
- Topical Retinoids
- Humidifiers
- Sunscreen
- Dietary Support
I have covered all these treatment factors in FAQ format. After reading, I hope you will learn more about the treatment of Ichthyosis.
1. What Is the Best Emollient and Moisturizer for Ichthyosis?
The best emollients and moisturizers for ichthyosis are those that deeply hydrate the skin, restore the skin barrier, and reduce scaling and dryness. Typically, products containing the following ingredients are recommended:
- Urea (5–20%): Helps to retain moisture in the skin while softening and reducing scaling.
- Ceramides: Crucial for repairing the skin barrier by replenishing natural lipids in the outermost layers of the skin.
- Lactic Acid or Alpha-Hydroxy Acids (AHAs): Mild exfoliants that remove dead skin cells and improve skin texture.
- Petrolatum-based Products (e.g., Vaseline): Act as occlusive agents, locking in moisture and protecting the skin from further irritation.
- Glycerin: A strong humectant that draws moisture into the skin and enhances hydration.
- Lanolin or Shea Butter: Provide deep moisturization and soothe cracked, irritated skin.
2. How Are Keratolytic Agents Used for Ichthyosis?
Keratolytic agents are an essential component of ichthyosis treatment because they help remove the accumulation of thick, scaly skin. These agents work by breaking down keratin in the outer layer of the skin, facilitating the shedding of dead skin cells and improving skin texture. Commonly used keratolytic agents include salicylic acid, urea, lactic acid, and alpha-hydroxy acids (AHAs).
3. How Is Bathing and Exfoliation Best for Ichthyosis?
Bathing and exfoliation play a crucial role in managing ichthyosis by helping to remove excess scales and improve skin hydration. Regular bathing in warm water softens the thickened skin and aids in loosening scales, making them easier to remove. Adding bath oils or emollients, such as colloidal oatmeal or mineral oil, to the water enhances skin hydration and prevents excessive dryness during bathing.
4. What Are Topical Retinoids Best for Ichthyosis?
Topical retinoids are best used for managing severe forms of ichthyosis, particularly when the condition involves excessive thickening of the skin. Retinoids, such as tretinoin or tazarotene, work by promoting cell turnover and reducing the buildup of keratin in the outer layers of the skin.
This action helps to thin the thickened scales and improve overall skin texture. Topical retinoids are especially beneficial in conditions like Lamellar Ichthyosis (LI) or Congenital Ichthyosiform Erythroderma (CIE) where scaling is pronounced.
5. Are Humidifiers Good for Ichthyosis?
Yes, humidifiers can be highly beneficial for individuals with ichthyosis. Maintaining adequate humidity levels in the indoor environment can help combat the excessive dryness and scaling characteristic of ichthyosis. Humidifiers work by adding moisture to the air, preventing the skin from losing too much water and reducing the risk of further drying or cracking.
6. Is Sunscreen Good for Ichthyosis?
Yes, sunscreen is beneficial for individuals with ichthyosis, particularly when their skin is exposed to sunlight. The condition often leaves the skin more vulnerable to irritation and damage, making sun protection essential. Broad-spectrum sunscreens with a high SPF (30 or above) help safeguard the skin from harmful UVA and UVB rays, reducing the risk of sunburn, dryness, and further damage to the already sensitive skin. Sunscreens containing hydrating ingredients, such as glycerin or ceramides, can offer additional moisture and barrier repair, which are advantageous for managing ichthyosis. It is recommended to use sunscreen free of fragrances or harsh chemicals to avoid exacerbating irritation. Regular application and reapplication as needed are key to ensuring effective protection.
7. Is Dietary Support Necessary for Ichthyosis?
Yes, dietary support can be beneficial for individuals with ichthyosis. A well-balanced diet rich in essential fatty acids, vitamins (such as A, D, and E), and antioxidants can support overall skin health and improve skin barrier function. Including foods like fish, nuts, seeds, and leafy greens may help reduce inflammation and dryness, complementing other treatment strategies for managing ichthyosis.
Disclaimer: The content provided in this document is for informational purposes only. It does not constitute medical advice.
: